Understanding sleep apnea involves recognizing how airway collapse occurs due to anatomical factors, neuromuscular control issues, and airway softness during sleep, leading to interrupted breathing and oxygen deprivation. Screening methods include questionnaires like the STOP-BANG, physical exams, and sleep studies such as polysomnography, which confirm diagnosis. Addressing these mechanisms and screening tools helps identify those at risk early, so you can learn more about effective detection and treatment options that could improve your sleep quality and overall health.
Key Takeaways
- Sleep apnea involves repeated airway collapses or obstructions during sleep, primarily caused by anatomical and neuromuscular factors.
- Obstructive sleep apnea results from airway blockage due to soft tissue or structural anomalies, while central sleep apnea involves brain signaling failures.
- Screening methods include polysomnography (sleep studies), home sleep apnea tests, and questionnaires like the STOP-BANG assessment.
- Advanced monitoring technologies utilize AI-driven devices and sensors to detect breathing irregularities and airway collapsibility.
- Identifying risk factors and symptoms early enables targeted diagnosis and personalized treatment approaches.
Understanding the Basic Mechanisms of Sleep Apnea
Sleep apnea occurs when your airway repeatedly collapses or becomes blocked during sleep, leading to interrupted breathing. Your sleep hygiene and sleep environment play essential roles in managing this condition. Poor sleep habits, such as irregular schedules or insufficient rest, can worsen airway collapse, while a disruptive sleep environment—like excessive noise, light, or uncomfortable bedding—can interfere with your breathing patterns. Ensuring a relaxing, quiet, and dark sleep space helps promote better airway stability. Maintaining consistent sleep routines reduces stress on your respiratory system, decreasing the likelihood of airway obstruction. Additionally, AI-driven security systems can monitor your sleep environment for disturbances, helping you identify and address factors that may contribute to apnea episodes. Sleep environment optimization also involves controlling temperature and humidity levels to prevent airway irritation. The use of air purifiers with HEPA filters can also improve indoor air quality, reducing irritants that might exacerbate breathing issues during sleep. By improving your sleep hygiene and optimizing your sleep environment, you support your body’s natural ability to keep the airway open, which can markedly reduce sleep apnea episodes and improve overall sleep quality.
Types of Sleep Apnea and Their Characteristics

There are three main types of sleep apnea, each distinguished by its underlying cause. Obstructive sleep apnea (OSA) is the most common, caused by a blockage in your airway during sleep. Central sleep apnea (CSA) occurs when your brain fails to send proper signals to your muscles that control breathing. Complex sleep apnea is a combination of both. Managing your sleep hygiene and sleep environment can help reduce symptoms, especially for OSA. Keeping your bedroom cool, dark, and quiet promotes better breathing. Avoiding alcohol and sedatives before bed also helps prevent airway relaxation. Additionally, building a backyard greenhouse can provide a relaxing environment that supports better sleep hygiene. Understanding these types allows you to tailor your approach to treatment and improve sleep quality. Recognizing the differences is key to addressing your specific sleep apnea type effectively. Incorporating exfoliation techniques such as gentle skin shedding may also improve skin health, which can influence overall well-being and sleep quality. Proper diagnosis and understanding of the vulnerabilities associated with each sleep apnea type enable more targeted and effective management strategies.
Anatomical Factors Contributing to Airway Collapse
Your airway’s structure plays a key role in sleep apnea. The position of your tongue, the shape of your jaw, and how your soft palate moves can all influence airway collapse during sleep. Understanding these factors helps identify why some people are more prone to breathing interruptions.
Tongue Position Impact
The position of the tongue plays an essential role in airway patency during sleep. Poor tongue posture, such as resting the tongue low or too far back, can obstruct the airway and worsen sleep apnea symptoms. A larger tongue size may also contribute to airway narrowing, especially during sleep when muscle tone decreases. When your tongue is positioned correctly—resting on the roof of your mouth and not blocking the throat—it helps keep the airway open. Conversely, a low or posterior tongue posture can cause the tongue to fall back into the airway, leading to partial or complete blockages. Maintaining good tongue posture and managing tongue size are fundamental for reducing airway collapse and improving sleep quality. Proper awareness of tongue position can aid in early screening and intervention strategies. Additionally, training methods that focus on tongue positioning can help strengthen muscles and support better airway maintenance during sleep. Techniques such as myofunctional therapy are increasingly being used to improve tongue posture and reduce sleep apnea symptoms.
Jaw Structure Variations
Variations in jaw structure considerably influence airway stability during sleep. If your jaw alignment is off, it can cause the airway to narrow or collapse, increasing the risk of sleep apnea. A misaligned jaw often leads to poor dental occlusion, which affects how your teeth fit together and can impact tongue positioning. When the jaw is recessed or disproportionate, it reduces the space available for airflow, making airway obstruction more likely. These anatomical differences are significant because they directly affect the potential for airway collapse during sleep. Recognizing jaw structure variations helps in evaluating sleep apnea risk and tailoring treatment options. Addressing jaw alignment issues, sometimes through orthodontic or surgical interventions, can improve airway patency and reduce symptoms.
Soft Palate Dynamics
Jaw structure influences airway stability, but the soft palate also plays a pivotal role in sleep apnea. Its elasticity determines how much it collapses during sleep, affecting airflow. A floppy soft palate with reduced elasticity can obstruct the airway, especially if the uvula is positioned low or hangs loosely. Uvula positioning varies among individuals and influences airway patency. When the soft palate relaxes excessively, it can cause airway narrowing or collapse. This dynamic behavior contributes markedly to obstructive sleep apnea episodes. Understanding soft palate mechanics helps identify risks and potential treatments. Consider this table for clarity:
| Feature | Description | Impact on Sleep Apnea |
|---|---|---|
| Soft palate elasticity | Flexibility of soft palate tissue | Higher elasticity reduces collapse |
| Uvula positioning | Uvula’s location and length | Low or elongated uvula increases risk |
| Soft palate thickness | Thickness influences stiffness | Thicker palate may resist collapse |
| Muscle tone | Muscle strength maintaining airway | Weak tone predisposes to collapse |
| Soft palate length | Length relative to airway | Longer soft palate can obstruct airway |
The Role of Neuromuscular Control in Maintaining Airway Patency
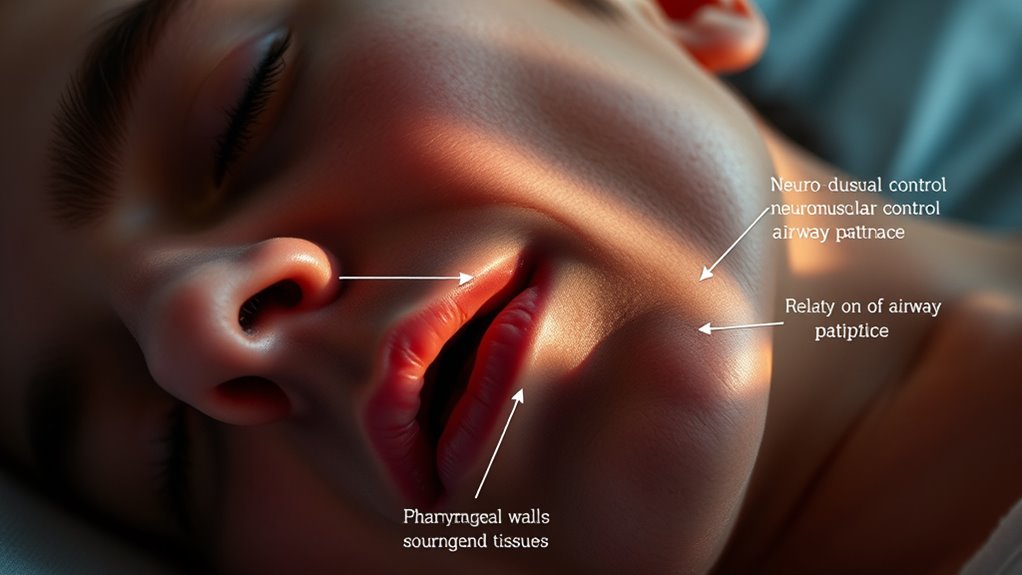
Your airway stays open thanks to neuromuscular control, which regulates muscle tone and prevents collapse. Factors like pharyngeal collapsibility and neural reflex mechanisms influence how effectively these muscles respond during sleep. Understanding these processes helps identify why some individuals are more prone to airway obstruction. Additionally, AI security vulnerabilities and the development of safety measures are crucial considerations in the ongoing enhancement of AI systems.
Muscle Tone Regulation
Neuromuscular control plays a crucial role in maintaining airway patency during sleep by regulating muscle tone in the upper airway. Your body continuously adjusts muscle tone regulation to keep the airway open, preventing collapse. When muscle tone is adequate, airway stabilization occurs, ensuring unobstructed airflow. During sleep, especially REM stages, this control diminishes, making it harder to maintain airway patency. Reduced muscle tone can lead to airway narrowing or collapse, contributing to sleep apnea events. You can influence this process through factors like body position and muscle activity. Maintaining proper neuromuscular control is essential for airway stability. Disruptions in muscle tone regulation compromise airway patency, which is a key factor in sleep apnea development and severity. Additionally, research shows that the decline in neuromuscular control during sleep is influenced by neuromuscular control mechanisms that can be affected by various physiological and lifestyle factors.
Pharyngeal Collapsibility Factors
The stability of the upper airway during sleep largely depends on the balance between the structural integrity of the pharyngeal walls and the neuromuscular control that supports them. When neuromuscular activity weakens, the airway becomes more collapsible, increasing airway resistance. This collapse often manifests as snoring, with higher snoring intensity indicating greater airway instability. Reduced neuromuscular tone allows the soft tissues to fall into the airway, narrowing it and making breathing more difficult. Factors like obesity, anatomical variations, or fatigue can impair neuromuscular responses, raising the likelihood of airway obstruction during sleep. Maintaining effective neuromuscular control is vital to prevent excessive collapsibility, reduce snoring intensity, and guarantee airway patency. This dynamic balance directly influences sleep quality and apnea severity.
Neural Reflex Mechanisms
Neural reflex mechanisms play a crucial role in maintaining airway patency during sleep by automatically modulating muscle activity in response to changes in airway patency. When your airway begins to narrow or collapse, neural reflexes are triggered to activate muscles that promote airway dilation. This reflexive neuromuscular control helps prevent airway obstruction, especially during sleep when voluntary muscle activation diminishes. Sensory receptors detect airflow disruptions and send signals to the brainstem, which then orchestrates rapid muscle responses. These reflexes ensure that airway muscles contract appropriately to keep the airway open, reducing the risk of apnea episodes. Without effective neural reflexes, airway collapsibility increases, heightening sleep apnea risk. This neuromuscular control is a key component in the body’s natural defense against airway obstruction during sleep.
Physiological Consequences of Repeated Airway Obstructions

Repeated airway obstructions during sleep trigger a cascade of physiological responses that can substantially impact your health. When your airway repeatedly collapses, your body experiences episodes of hypoxia, leading to hypoxia-induced damage at the cellular level. This lack of oxygen stresses your cardiovascular system, increasing blood pressure and causing your heart to work harder. Over time, these repeated events can contribute to hypertension, arrhythmias, and other cardiovascular effects. The sudden drops in oxygen levels also activate sympathetic nervous system responses, raising your heart rate and constricting blood vessels. These chronic changes elevate your risk for heart disease and stroke. Additionally, AI technologies are increasingly utilized to detect sleep apnea patterns, facilitating early diagnosis and treatment. Recognizing the role of physiological responses in sleep apnea can further improve screening strategies and patient outcomes. Understanding these physiological consequences underscores the importance of recognizing and treating sleep apnea early to protect your long-term health. Moreover, ongoing research continues to explore the impacts of intermittent hypoxia, highlighting the importance of effective management strategies.
Progression and Complications Associated With Sleep Apnea

As sleep apnea progresses without treatment, the repeated episodes of airway obstruction can lead to increasingly severe health complications. You may experience chronic sleep deprivation, which affects your mood, concentration, and overall well-being. Over time, this can result in:
- Elevated risk of cardiovascular issues like hypertension and heart disease
- Increased chances of type 2 diabetes due to disrupted metabolism
- Impaired cognitive function and memory problems
- Greater difficulty in making effective lifestyle modifications, perpetuating the cycle. Monitoring symptoms is crucial to prevent further health deterioration. Recognizing the progression of sleep apnea can help facilitate early intervention and improve long-term health outcomes.
Ignoring these progression signs can worsen your health. Addressing sleep apnea early helps reduce sleep deprivation and promotes lifestyle changes that support better breathing. Recognizing these complications emphasizes the importance of timely intervention.
Clinical Screening Tools and Questionnaires for Identifying Risk

Clinical screening tools and questionnaires play a crucial role in identifying individuals at risk for sleep apnea before confirmatory testing. They help you recognize common signs like loud snoring and daytime fatigue, which are key indicators of potential sleep disruption. The STOP-Bang questionnaire is widely used, asking about snoring, tiredness, observed apneas, high blood pressure, BMI, age, neck circumference, and gender. Similarly, the Epworth Sleepiness Scale measures how likely you are to doze off during daily activities, highlighting daytime fatigue. These tools are quick, non-invasive, and effective at screening large populations. While they don’t confirm sleep apnea, they guide you toward seeking further testing. Using these questionnaires, you can identify symptoms early and improve your chances of getting timely diagnosis and treatment.
Advanced Diagnostic Tests for Confirming Sleep Apnea

To definitively diagnose sleep apnea, advanced diagnostic tests are essential, as they provide objective data that surpass the limitations of screening questionnaires. These tests include:
- Advanced imaging like MRI or CT scans, which reveal detailed airway structures and obstructions.
- Polysomnography (sleep study), the gold standard, measuring brain activity, breathing, and oxygen levels overnight.
- Genetic testing, identifying inherited predispositions that may contribute to sleep apnea risk.
- Home sleep testing devices, offering a less invasive way to gather extensive respiratory data.
- Regular monitoring of indoor air quality can help identify environmental factors that may exacerbate sleep disturbances and respiratory issues.
These methods help clarify the underlying causes, guide treatment plans, and ensure accurate diagnosis beyond subjective assessments. Using advanced imaging and genetic insights, you gain a clearer picture of your sleep disorder’s root.
Frequently Asked Questions
How Does Sleep Position Influence Sleep Apnea Severity?
Your sleep position plays a big role in sleep apnea severity. When you sleep on your back, gravity can cause your airway to collapse more easily, worsening symptoms. By using positional therapy and adjusting your sleep posture—like sleeping on your side—you can reduce apnea episodes. Consistently maintaining good sleep posture helps lessen severity, making your sleep more restful and improving overall health.
Can Lifestyle Changes Fully Reverse Sleep Apnea?
Did you know that nearly 50% of sleep apnea cases improve with lifestyle changes? While lifestyle modifications and weight management can substantially reduce symptoms, they might not fully reverse sleep apnea for everyone. You can often see improvements, but severe cases may still require medical interventions like CPAP. Staying committed to healthy habits can make a big difference, yet consulting a healthcare professional remains essential for personalized treatment.
What Genetic Factors Contribute to Sleep Apnea Risk?
You might wonder about genetic factors influencing sleep apnea risk. Genetic predisposition plays a significant role, as your genes can affect airway size and muscle tone. Familial clustering shows that sleep apnea often runs in families, indicating inherited traits increase your susceptibility. While lifestyle changes help manage symptoms, understanding your genetic background can guide personalized prevention and treatment strategies, making you better equipped to address the condition proactively.
How Do Comorbid Conditions Affect Sleep Apnea Diagnosis?
Comorbid conditions profoundly influence sleep apnea diagnosis by creating diagnostic challenges. When you have other health issues like obesity, hypertension, or heart disease, symptoms may overlap or mask sleep apnea signs, making it harder to identify. This comorbid influence can delay diagnosis or lead to misdiagnosis, so it’s vital to take these conditions into account carefully and use thorough screening methods. Addressing comorbidities improves accuracy and guarantees appropriate treatment.
Are There Emerging Technologies Improving Sleep Apnea Detection?
Imagine slipping on a sleek wearable device that feels like a second skin, seamlessly capturing your sleep patterns. Emerging technologies like advanced home testing and wearable devices make detecting sleep apnea easier and more accessible. These innovations provide real-time data, allowing you to monitor your breathing and sleep quality from the comfort of your home. As technology advances, you gain more accurate, convenient tools to identify and address sleep apnea early on.
Conclusion
Understanding sleep apnea’s complex mechanisms helps you recognize its signs and risks. By knowing the anatomical and physiological factors involved, you can better identify who may need further testing. Don’t forget, even in this modern age, some clues are as old as the landline—like snoring or daytime fatigue—that warrant attention. Staying vigilant and using proper screening tools guarantees you don’t miss the chance to prevent serious health complications. Sleep well, and don’t let sleep apnea be your unwelcome guest.









