Bioprinting organs could revolutionize transplantation by offering custom, lab-grown replacements tailored to your needs. It promises to reduce waiting times and eliminate organ shortages, but many challenges remain, like replicating complex structures and ensuring proper blood flow. Ethical questions about materials and accessibility also arise. If you want to discover how this innovative field might reshape healthcare and what hurdles still exist, there’s much more to explore.
Key Takeaways
- Bioprinting enables the creation of lab-grown, patient-specific organs to potentially eliminate transplant waiting lists.
- Advances focus on developing complex tissue structures and vascular systems essential for functional organ integration.
- Ethical concerns include tissue sourcing, consent, ownership rights, and preventing misuse for non-therapeutic purposes.
- Technological challenges involve perfecting bioinks, printer precision, and ensuring organ functionality and immune compatibility.
- Responsible progress in bioprinting could revolutionize transplantation, making organ shortages a thing of the past.

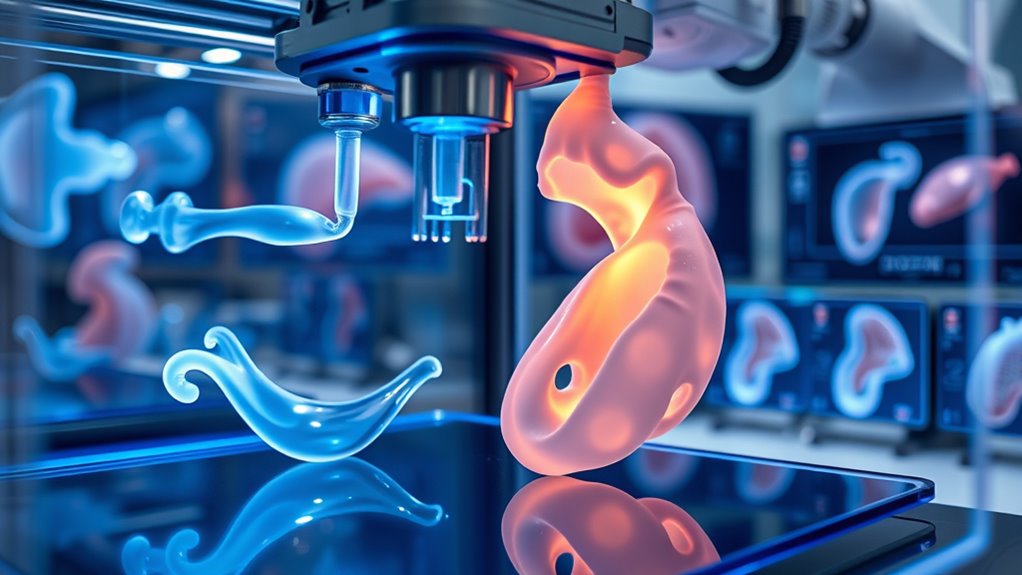
Have you ever wondered how science is revolutionizing medicine? One of the most exciting advancements is bioprinting organs, which promises to transform transplantation and save countless lives. Instead of waiting years for donor organs, you could soon benefit from lab-grown replacements tailored precisely to your body. But as remarkable as this technology is, it also raises important questions about ethical considerations and technological challenges that need to be addressed before it becomes a routine medical option.
When you think about ethical considerations, it’s essential to recognize the complex issues surrounding bioprinting. For example, questions about the source of biological materials come to the forefront. If tissues or cells are derived from donors, consent and ownership rights become important topics. Furthermore, the idea of creating fully functional organs raises concerns about potential misuse, such as creating organs for non-therapeutic purposes or even “designer” organs with enhanced abilities. Society must carefully weigh the benefits of this technology against potential moral dilemmas, guaranteeing that bioprinting is used responsibly and fairly. The debate also touches on issues of accessibility—who will have access to these organs, and how can equitable distribution be guaranteed? These ethical issues are essential to address alongside technological progress to prevent misuse and guarantee the technology benefits everyone.
On the technological side, you face significant challenges in making bioprinting a reliable, safe, and practical process. Creating functional organs isn’t just about stacking cells; it requires replicating the complex architecture and vascular systems that keep organs alive and functioning. Achieving this level of precision demands cutting-edge bioprinters capable of handling delicate biological materials without damaging them. Additionally, developing suitable bioinks—materials that can mimic natural tissue—poses a major hurdle. These bioinks must support cell growth, be biocompatible, and eventually integrate seamlessly with the patient’s body. Guaranteeing the printed organs develop proper blood flow, nerve connections, and immune acceptance remains a daunting task. Researchers are continuously working on overcoming these technological challenges, but it’s a process that takes time and rigorous testing. Improving bioink formulations and printer precision is crucial for success. Overcoming these barriers is critical for bioprinting to transition from experimental labs to everyday clinics.
Despite these hurdles, the potential benefits of bioprinting organs are undeniable. If the ethical considerations are thoughtfully managed and the technological challenges overcome, you could see a future where organ shortages are a thing of the past. For now, the journey involves balancing innovation with responsibility, making sure this groundbreaking science advances safely and ethically. The promise of seeing your own personalized, lab-grown organ replace a failing one is inspiring—just remember, it’s a future built on careful progress and thoughtful reflection.

Bioprinting: Techniques and Risks for Regenerative Medicine
As an affiliate, we earn on qualifying purchases.
As an affiliate, we earn on qualifying purchases.
Frequently Asked Questions
How Long Does It Take to Bioprint an Entire Organ?
It typically takes several hours to a few days to bioprint an entire organ, depending on its complexity and printing speed. You need to guarantee proper organ maturity, so the bioprinting process allows for cell growth and development afterward. Faster printing speeds can cut down production time, but maintaining precision and cell viability is essential. Overall, the process balances speed with quality to create functional, transplant-ready organs.
What Are the Primary Ethical Concerns Surrounding Organ Bioprinting?
You might think organ bioprinting raises only technical issues, but ethical concerns are just as crucial. Ensuring informed consent is vital, so patients understand the risks involved. Additionally, you should consider equitable access—avoiding a future where only the wealthy benefit. These concerns highlight the need for regulations that protect individuals and promote fairness, ensuring bioprinting advances serve everyone, not just a privileged few.
Can Bioprinted Organs Fully Mimic Natural Organ Functions?
Bioprinted organs can’t yet fully mimic natural organ functionality due to current bioprinting limitations. While advancements improve tissue complexity, you may find that bioprinted organs lack the intricate cell interactions and vascular networks essential for complete function. These limitations mean bioprinted organs are promising but still require further development to match the performance of natural organs, so you should stay informed about ongoing research and innovations.
What Are the Current Regulatory Challenges in Organ Bioprinting?
Ever wonder how we navigate the complex regulatory landscape? You face challenges like defining clear pathways for approval, ensuring safety, and addressing intellectual property rights. Regulatory agencies struggle to keep pace with rapidly advancing bioprinting tech, making standardization difficult. You need to contemplate how to protect innovations while establishing guidelines that guarantee patient safety. These hurdles slow down bringing bioprinted organs from lab to clinic, demanding collaborative efforts for streamlined regulations.
How Scalable Is the Bioprinting Technology for Widespread Clinical Use?
You can expect bioprinting technology to become more scalable for widespread clinical use, but challenges remain. Achieving cost efficiency is vital, and current material limitations hinder printing complex, durable organs. As research advances, you’ll see improvements in bioprintable materials and production methods, making organ bioprinting more practical. Nonetheless, scaling up will require overcoming these obstacles to guarantee safe, affordable, and reliable organ replacements for many patients.

Hydrogels and Bioinks in Tissue Engineering (Biological and Medical Physics, Biomedical Engineering)
As an affiliate, we earn on qualifying purchases.
As an affiliate, we earn on qualifying purchases.
Conclusion
Imagine a world where damaged organs fade away, replaced by living, breathing tissues crafted just for you. As bioprinting advances, you could walk into a future where your body’s missing parts are seamlessly restored, like a master artist filling in a blank canvas. No more waiting, no more rejection—just vibrant, perfectly suited organs growing inside you. This is the promise of bioprinting, turning science fiction into life-saving reality before your very eyes.

3D Bioprinting: Fundamentals, Principles and Applications
As an affiliate, we earn on qualifying purchases.
As an affiliate, we earn on qualifying purchases.

Synthetic Biology Startups: Monetize CRISPR, Lab-Grown Organs, and Biohacking by 2030
As an affiliate, we earn on qualifying purchases.
As an affiliate, we earn on qualifying purchases.