Fertility awareness methods (FAMs) help you identify fertile days by tracking signs like basal body temperature and cervical mucus changes, which are driven by hormonal shifts such as estrogen, LH, and progesterone. Their effectiveness depends on consistent observation, understanding of cycle patterns, and diligent record-keeping. While nearly 76-99% effective with perfect use, typical use can be less reliable. To discover more about how these signs work and improve your accuracy, keep exploring the physiological principles behind FAMs.
Key Takeaways
- FAMs track physiological signs like basal body temperature and cervical mucus to identify fertile windows with effectiveness varying by user consistency.
- Ovulation causes hormonal changes: increased estrogen and LH lead to cervical mucus changes, while progesterone rise post-ovulation slightly raises BBT.
- Consistent daily monitoring of BBT and mucus enhances accuracy in detecting ovulation and understanding fertility patterns.
- Proper education and diligent record-keeping improve the efficacy of FAMs, though irregular cycles may pose challenges.
- Technological tools and algorithms support interpretation of hormonal and physiological data, increasing reliability of fertility predictions.
Understanding Fertility Awareness Methods and Their Types
Fertility awareness methods (FAMs) are natural approaches that help you identify your most fertile days by tracking your body’s signs of ovulation. Many people encounter fertility myths that can create confusion or false hopes, so understanding the facts is essential. These methods vary, including tracking basal body temperature, cervical mucus, and calendar cycles. FAMs empower you to take control of your reproductive health without medications or devices. They also encourage open dialogue and vulnerability with your partner, which can improve mutual understanding and support when navigating fertility. However, the emotional impacts can be mixed; some may feel more connected to their bodies, while others might experience anxiety if cycles aren’t regular. Knowing the different types of FAMs helps you choose a method suited to your lifestyle, ensuring you’re better prepared for pregnancy planning or natural family planning. Additionally, understanding the accuracy of these methods can help set realistic expectations and improve their effectiveness. Being aware of safe sleep environments and managing sleep deprivation can further support overall reproductive health and well-being.
How Physiological Signs Indicate Fertile and Infertile Days
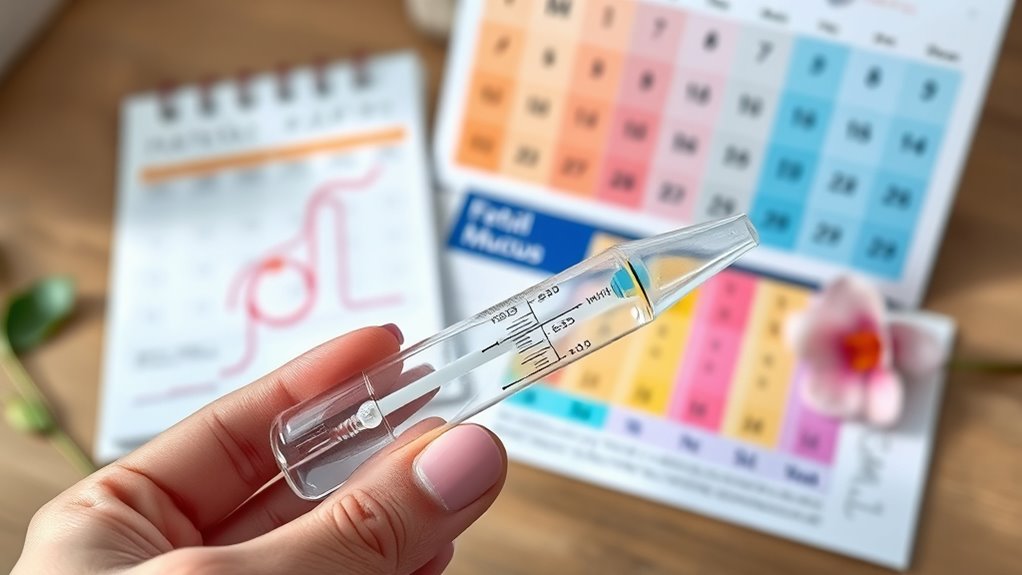
You can identify fertile days by noticing changes in your cervical mucus, which becomes clear and stretchy. Monitoring your basal body temperature each morning also helps reveal when you’re most fertile, as it slightly rises during ovulation. By paying close attention to these signs, you gain valuable insights into your reproductive cycle. Additionally, understanding physiological signs helps in accurately tracking fertility windows, especially when considering ovulation timing and other biological cues. Recognizing protective styling benefits can also aid in maintaining healthy hair during this cycle.
Detecting Cervical Mucus Changes
Detecting cervical mucus changes is a key way to identify your fertile and infertile days. By observing cervical mucus consistency, you can pinpoint when ovulation is approaching and occurring. During fertile days, mucus becomes clear, stretchy, and egg white-like, which is ideal for mucus ovulation detection. This change signals increased estrogen levels and indicates your most fertile window. In contrast, infertile days typically feature dry or sticky mucus, showing lower estrogen activity. Regularly checking cervical mucus allows you to track these patterns accurately. Pay attention to how the mucus feels and looks each day; this physiological sign provides reliable clues about your fertility status. Additionally, understanding hormonal fluctuations helps explain why these mucus changes occur and enhances your ability to interpret your signs correctly. Recognizing cycle patterns can help you better predict your fertility window and plan accordingly. Monitoring mucus changes is especially useful because it offers a non-invasive way to observe your body’s natural signs of fertility, aligning closely with biological processes that regulate ovulation. Using mucus changes as part of your fertility awareness method helps you better understand your cycle without invasive procedures.
Monitoring Basal Body Temperature
Monitoring basal body temperature (BBT) involves taking your temperature at the same time every morning before getting out of bed. This consistent habit helps you identify ovulation timing by tracking temperature fluctuations throughout your cycle. Typically, you’ll notice a slight rise in BBT—about 0.2 to 0.5°F—after ovulation occurs. This temperature shift marks the changeover from infertile to fertile days. By recording your daily temperatures, you can pinpoint when ovulation happens, making it easier to understand your cycle. Recognizing these physiological signs allows you to determine your fertile window more accurately. Over time, patterns in temperature fluctuations reveal your ovulation pattern, helping you plan or prevent pregnancy based on your body’s natural rhythms. Additionally, understanding angel number meanings can provide spiritual insight into your fertility journey.
The Science Behind Basal Body Temperature Tracking

Understanding the science behind basal body temperature (BBT) tracking involves recognizing how hormonal changes influence your body’s internal heat. As you approach ovulation, estrogen levels rise, keeping your temperature relatively low. After ovulation, the hormone progesterone increases, causing a slight but noticeable rise in your BBT—about 0.2 to 0.5°F. This temperature variation helps with ovulation prediction, indicating when you’ve just ovulated. Tracking these fluctuations daily allows you to identify your fertile window accurately. The key is consistency, as even minor deviations can mask the temperature shift. By understanding how hormonal shifts affect your basal temperature, you gain a physiological insight into your cycle, making BBT an effective tool for fertility awareness and planning. Additionally, knowing how to interpret these changes can improve your overall homesteading skills related to health and wellness. Regular monitoring can also help you notice other health patterns that may influence your reproductive health.
The Role of Cervical Mucus in Fertility Monitoring

Cervical mucus plays an essential role in fertility awareness because its changes reflect hormonal shifts that signal your most fertile days. You can observe these changes through mucus observation techniques, which involve checking the consistency, color, and stretchiness of your cervical mucus daily. During your fertile window, your mucus becomes clear, stretchy, and egg-white-like, indicating high fertility. Outside this period, mucus may be thick, sticky, or absent, signaling lower fertility. Paying attention to cervical mucus consistency helps you identify your peak fertility days accurately. Consistent observation and recording allow you to detect patterns over time. This non-invasive method provides valuable insights into your body’s natural signs of fertility, making it a reliable component of fertility awareness methods.
Hormonal Patterns and Their Significance in Fertility Awareness

Understanding your hormonal patterns is key to fertility awareness, as these fluctuations signal your most fertile days. You’ll notice specific changes in key hormones like estrogen and progesterone throughout your menstrual cycle. Recognizing these patterns helps you better interpret your body’s signs and plan accordingly.
Menstrual Cycle Hormonal Fluctuations
Hormonal fluctuations during your menstrual cycle play a crucial role in fertility awareness because they directly influence ovulation and other signs of fertility. These fluctuations result from hormonal regulation that occurs across different menstrual cycle phases. During the follicular phase, levels of estrogen rise, signaling the body to prepare for ovulation. Near mid-cycle, a surge in luteinizing hormone triggers the release of an egg. In the luteal phase, progesterone increases to support a potential pregnancy. If fertilization doesn’t occur, hormone levels decrease, leading to menstruation. Understanding these hormonal patterns helps you identify fertile days and track your cycle accurately. Recognizing how hormonal regulation shifts through the menstrual cycle phases enhances your ability to utilize fertility awareness methods effectively. Additionally, automation’s role in analyzing hormonal data can improve the accuracy of fertility tracking tools, especially when integrated with personal health data and advanced algorithms.
Key Hormones in Fertility
Key hormones such as estrogen, progesterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH) drive the changes in your menstrual cycle that determine fertility. These hormones regulate the hormonal patterns essential for ovulation timing and overall cycle health. Estrogen peaks to thicken the uterine lining and signal the approaching ovulation, while a surge in LH triggers ovulation itself. FSH stimulates follicle development, preparing an egg for release. After ovulation, progesterone levels rise, maintaining the uterine lining for possible pregnancy. Understanding hormonal regulation helps you identify fertile windows accurately. Tracking these key hormones’ patterns allows you to determine ovulation timing, which is vital for fertility awareness and planning. Consistent observation of hormonal signals offers insight into your cycle’s fertility phases. Additionally, monitoring hormonal fluctuations can provide more precise information about your reproductive health, highlighting the importance of hormone pattern tracking in fertility awareness.
Evaluating the Effectiveness and Limitations of FAMs

Evaluating the effectiveness and limitations of Fertility Awareness Methods (FAMs) requires examining how accurately they predict ovulation and prevent pregnancy. While FAMs can be effective when used correctly, their effectiveness heavily depends on user compliance and consistency. Common limitations include difficulty tracking fertility signs daily, hormonal fluctuations that may cause misleading readings, and the need for diligent record-keeping. Additionally, effectiveness limitations arise if you forget to check your signs or misinterpret data. Here are key points to consider:
- User compliance is essential for accuracy.
- Variability in fertility signs can cause errors.
- FAMs may be less effective during irregular cycles.
- Proper education and consistent use improve reliability.
- Fertility monitoring techniques such as creating designated zones can help organize fertility tracking tools and records for better adherence.
- Incorporating hormonal fluctuations awareness into tracking can further improve the reliability of fertility assessments.
Frequently Asked Questions
How Do Lifestyle Factors Affect Fertility Awareness Method Accuracy?
Lifestyle factors can critically impact the accuracy of fertility awareness methods. Hormonal fluctuations caused by stress, poor sleep, or diet changes can make it harder to identify your fertile window accurately. Stress management is essential, as high stress levels may distort hormonal signals. By maintaining a healthy lifestyle, you help keep hormonal patterns stable, improving your ability to track fertility signs reliably and making your fertility awareness method more effective.
Can Fertility Awareness Methods Be Used Postpartum or During Breastfeeding?
Thinking of postpartum fertility as a delicate garden, you’ll find it tricky to rely solely on fertility awareness methods during breastfeeding. Postpartum fertility fluctuates, especially with breastfeeding challenges that suppress ovulation unpredictably. While some women can track fertility signs, hormonal changes make these methods less reliable during this period. So, if you want certainty, consider additional contraception methods, as breastfeeding alone might not be enough to guard against an unplanned pregnancy.
Are There Specific Age Groups Where FAMS Are More Reliable?
You might wonder if age-related fertility affects FAM reliability. Generally, FAMs are more reliable for women in their 20s and early 30s, when fertility patterns are more predictable. As you age, especially after 35, fertility varies more, leading to reliability variations. So, your age can influence how accurately FAMs reflect your fertility status, making them less dependable for older women or those with irregular cycles.
How Do Medications Influence Fertility Signs and Tracking?
Oh, joy! Medications love to play havoc with your fertility signs, don’t they? Hormonal interference and medication side effects can make tracking tricky, as they mess with basal body temperature, cervical mucus, and cycle patterns. You might think you’re in sync, but your meds could be secretly throwing off your signals. Always check with your doctor, because your body’s whispers might be drowned out by pharmaceutical noise.
What Are the Emotional Impacts of Using Fertility Awareness Methods?
Using fertility awareness methods can profoundly impact your emotional well-being, as tracking your fertility signs may lead to feelings of empowerment or anxiety. It might also influence your relationship dynamics, encouraging open communication or creating stress if insecurities arise. You could experience a mix of confidence and frustration, depending on your success with tracking. Staying mindful of these emotions helps you navigate the process more positively and maintain healthy connections.
Conclusion
Fertility awareness methods can be highly effective when you understand your body’s signs. For example, tracking basal body temperature and cervical mucus can help you identify fertile days accurately. Did you know that with perfect use, FAMs have a typical use failure rate of about 2%? This shows they’re a reliable natural option if you’re consistent and attentive. Just remember, understanding your body’s signals is key to making FAMs work best for you.








